Bioarchaeology International
Volume 6, Numbers 1–2: 23–40
DOI: 10.5744/bi.2021.0003
Received 19 January 2021
Revised 10 September 2021
Accepted 19 September 2021
Beyond Mortality: Survivors of Epidemic Infections and the Bioarchaeology of Impairment and Disability
Heather T. Battlesa* and Rebecca J. Gilmourb
ABSTRACT Epidemics and pandemics are typically discussed in terms of morbidity and mortality, susceptibility and immunity, and social responses to and impacts of the immediate epidemic event. Much less attention is paid to the longer-term consequences for individuals and populations in terms of the sequelae of infections, such as blindness after smallpox, deafness due to congenital rubella, and paralysis after polio. This same tendency is observed in the COVID-19 pandemic, with counts of cases and deaths, questions of immunity, and economic impacts at the foreground and long-term or chronic health impairment of COVID-19 survivors receiving less attention. Much of the existing research on the effects of such disease sequelae has come from disability history; in addition, the bioarchaeology of impairment/disability is an emerging area of research that can contribute insight into experiences of disease consequences. In this article, we give an overview of published work on survivors of infectious disease using both bioarchaeology and disability history. Using the example of post-polio paralysis, we propose a theoretical approach to the bioarchaeological study of infectious disease that is inclusive of the history of impairment and disability, which we refer to as a survivor lens. We structure this discussion through scaffolded questions that move through multiple levels of analysis: from the individual and relational to the drivers of cultural change. We argue that bioarchaeological research on past epidemics and pandemics that attends to morbidity, lasting impairment, and disability can contribute to wider conversations about infectious disease and disability in the past and present.
Keywords: sequelae; poliomyelitis; palaeopathology
En général, les épidémies et les pandémies sont considérées en termes de morbidité et de mortalité, de susceptibilité et d’immunité, et de réponses sociales et d’impacts immédiats de l’événement épidémique. Moins d’attention est accordée aux conséquences à long terme pour les individus et les populations en termes de séquelles d’infections, telles que la cécité après la variole, la surdité due à la rubéole congénitale et la paralysie après la polio. Cette même tendance est observée lors de la pandémie de COVID-19. Il y a moins d’attention accordée au nombre de cas et de décès, aux questions d’immunité et d’impacts économiques au premier plan, et aux problèmes de santé à long terme ou chroniques des survivants de COVID-19 reçoivent. Une grande partie de la recherche existante sur les effets de ces séquelles de la maladie provient de la recherche sur les déficiences/handicaps. De plus, la bioarchéologie de la déficience/handicap est un domaine de recherche émergent qui peut contribuer à mieux comprendre les expériences des conséquences de maladie. Dans cet article, nous donnons un aperçu des travaux publiés sur les survivants de maladies infectieuses en utilisant à la fois la bioarchéologie et l’histoire du handicap. En utilisant l’exemple de la paralysie post-polio, nous proposons une approche théorique de l’étude bioarchéologique des maladies infectieuses qui inclut l’histoire de la déficience/handicap, que nous appelons une lentille de survivant. Nous structurons cette discussion à travers des questions échafaudées qui traversent de multiples niveaux d’analyse: de l’individu au relationnel, jusqu’au aux changements culturels. Nous soutenons que la recherche bioarchéologique sur les épidémies et pandémies historiques qui examine la morbidité et le handicap peut contribuer à des conversations plus larges sur les maladies infectieuses et le handicap au passé ainsi qu’au présent.
Mots clés: séquelles; poliomyélite; paléopathologie
Bioarchaeologists have undertaken considerable study on past epidemics, including, most frequently, plagues caused by the bacterium Yersinia pestis (e.g., DeWitte 2014; Spyrou et al. 2019). Many of these studies have contributed extremely valuable insight into the vulnerability and risk of different demographic groups in societies, primarily in Europe (e.g., Castex and Kacki 2016; DeWitte 2009, 2010; DeWitte and Wood 2008; Godde et al. 2020; Kacki and Castex 2014; Rigeade et al. 2009; Signoli et al. 2007; see also critical review by Bramanti et al. 2018). Due to the nature of the Y. pestis pathogen, these investigations looked at people who succumbed relatively quickly. Accordingly, bioarchaeologists often focus their studies on larger cemetery/burial deposits associated with mass deaths from epidemics of this and other infectious diseases. But in addition to the individuals who died of these diseases, there was also a portion of individuals who survived them. For example, while smallpox is notoriously deadly, 65% to 80% of infected people would have actually survived this condition, albeit frequently with long-term sequelae (long-term biological consequences of infection) (Semba 2003). Up to 9% of smallpox cases developed ocular complications (e.g., corneal ulcers) or severe scarring around the eye, making that disease the leading cause of blindness in Europe in the centuries preceding inoculation (Semba 2003). While some consequences of epidemic disease that survivors experienced may be visible archaeologically, much of the evidence may be too nonspecific to identify a clear “survivor cohort” (i.e., those who contracted but did not die of the disease). However, we argue that simply remembering that these survivors exist can provide bioarchaeologists with new approaches and lenses through which to understand the lasting repercussions of epidemics, some of which we discuss here. Additionally, such an approach could potentially assist in the (re)interpretation of palaeopathological features in well-dated assemblages.
In this article, we define a survivor as someone who has lived through the acute stage of an epidemic infection, whether or not the pathogen is cleared from the body (e.g., measles) or persists in a latent form (e.g., varicella-zoster or tuberculosis) with potential for later reactivation. These survivors might or might not experience lasting effects of that infection, but they are nevertheless part of a larger group of people who contracted an epidemic disease but did not die of it. Recognizing that the observation of skeletal changes associated with disease is something palaeopathologists already do, what we are proposing is a particular theoretical (rather than methodological) perspective that, when integrated in study designs and interpretations, can not only add to our understanding of the past but also contribute to bringing bioarchaeological work into wider conversations about the impacts of epidemics and pandemics in the present and future.
Amid the current COVID-19 pandemic (2019–present), much focus has been placed on 1) deaths and counts of deaths (the death toll), 2) risk factors for disease-associated mortality at the personal level (e.g., obesity, asthma), and 3) disparities in COVID-19 mortality among racialized and marginalized groups. However, Long COVID also emerged early on as a concern, as COVID-19 survivors suffering from lasting effects of the disease (aka “long-haulers”) sought to raise awareness (see Perego et al. 2020), in the hopes of ending stigma and prompting more medical research toward possible treatments. Long COVID has brought to mind the sequelae of other diseases, such as neurological disorders following influenza (Honigsbaum and Krishnan 2020), cognitive impairment following cerebral malaria (John et al. 2008), and eyesight and hearing loss consequent to infection with Ebola virus (Clark et al. 2015). Furthermore, new research around post–COVID-19 sequelae has highlighted how medical interventions such as mechanical ventilation and life support have their own associated potential sequelae (Torres-Casto et al. 2021; for physical impairments associated with post–intensive care syndrome, see Ohtake et al. 2018). Despite neurological involvement and potential resulting sequelae, for example, being common in epidemics and pandemics, these complications and chronic illnesses are underrecognized and understudied—with even less attention paid to their personal, social, and economic consequences (Valerio et al. 2020).
Poliomyelitis (polio for short), however, is an example of a disease better known for its long-term impact on survivors (hence its older name, “infantile paralysis”) than for its mortality rate. Polio in the twentieth century was also deeply connected to the disability rights movement, through polio survivors. In this article, we use polio to illustrate post-epidemic survivorship and ground our discussion regarding this theoretical approach. We argue that although great focus has been placed on epidemic mortality due to its implications for demography and host–pathogen evolution (among other major topics in biological anthropology), the epidemic survivor cohort should not be forgotten in bioarchaeological contexts. In our infectious disease examples, it is clear that disease sequelae encountered by survivors may considerably affect their post-epidemic experiences through physical impairments as well as social stigma. While skeletal evidence for infectious disease sequelae is regularly described in the form of bioarchaeological case studies, we suggest that, when appropriate, these individuals should also be seen as part of a larger, “long-hauler” group affected by epidemic infectious disease. Adopting this “survivor lens,” which integrates epidemic and disability research, can allow researchers to consider impacts on individuals, their relations (e.g., their families/households), and societies. Through the use of a survivor lens, we argue that bioarchaeologists can ask appropriate questions about individuals and their bodies, place those bodies within social landscapes, and consider the larger cultural changes that may be linked to survivor cohorts following epidemics. Accordingly, it can contribute to efforts to grow bioarchaeological approaches from traditional case studies to group-level investigations of social experience (for discussion of progress in this area, see Buikstra and Roberts 2012).
Infectious Disease Survivors in Disability History
While it is true that disability can exist without disease, and vice versa, the two have had an intimate relationship for centuries, and in some cases they are inextricably linked. Linker (2013:505)
Disability history emerged out of the civil rights struggles that, by the 1980s, launched the field of disability studies. Disability activists wanted to shift the focus from physical impairment to social disablement in order to direct attention to the political, rather than the personal and the medical (Oliver 1996; see UPIAS and the Disability Alliance 1975; Disabled Peoples’ International 1981; for a discussion of this history, see also Hurst 2005). Out of this came the medical (or individual) and social models of disability, which distinguish the medicalization of disability from the activists’ perspective of disability as a social situation arising from discrimination and prejudice, and not from the impairment itself. The medical model defines disability based on biological dysfunction (i.e., impairment), with a focus on treatment and “cure,” relegating issues to hospitals, clinics, and individual health interactions under the medical gaze, with medical solutions. As such, those operating according to the medical model tend to use the term “disability” interchangeably with “impairment” to describe compromised physical and/or cognitive function (Rothman 2010; Shakespeare 2012). In contrast, the social model holds that disability is caused solely by exclusionary social and physical structures; individuals with impairments are not “disabled” by their biology, but rather by the discriminatory, oppressive, and stigmatizing behaviors and environments within society (Llewellyn and Hogan 2000). Under the social model, “impairment” and “disability” are distinct and separate concepts.
In the first decades of the twenty-first century, critiques of the social model emerged that called for complicating the strict binary of impairment versus disability (for a review and discussion, see Rembis 2019). Under proposed alternative approaches, the medical and social models are still important and useful—but not mutually exclusive. Snyder and Mitchell’s (2010) “cultural” model, for example, accounts for both the lived reality of a compromised biological state as well as the disabling impacts of marginalizing social and physical environments. This approach recognizes the constructed nature of the body and identity, preserving the role of biological impairment in contrast to its rejection under the social model (Snyder and Mitchell 2010). Physiological impairments experienced by disabled people (the term according to identity-first language, increasingly preferred by many disability communities, as opposed to “people with disabilities,” the term according to people-first language) likely comprise an important aspect of their embodied identities, which play a role in the disadvantages they encounter and contribute to how they experience their world (Shakespeare 2012).
As biosocial/biocultural anthropologists readily recognize, the biological and the social/cultural are deeply intertwined (Fuentes 2020; Shakespeare 2014). We cannot deny the role that the body and physical experiences play in an individual’s lived experience and sociocultural context; impairments may indeed shape how social and cultural situations are experienced. Furthermore, impairment and disability are dynamic, situated, and intersectional with age, gender, race, religion, class, and other markers of identity (Rembis 2019). Accepting impairment/disability as overlapping and interrelated categories allows for more complexity and nuance in considering pain and suffering, as well as more critical engagement—but not rejection—of concepts such as diagnosis, treatment, recovery, cure, and care (Rembis 2019). The emergence of these alternative approaches and their associated critiques of the social model should not be perceived as a rejection of the social model per se but rather as a sign of its extraordinary influence and usefulness in moving understandings of disability forward. By breaking the assumed link between physical impairment and social disability, the social model de-naturalized disability and opened up space for not only changing policy and professional practice but “transform[ing] consciousness” more broadly (Oliver 1996:42). This reconceptualization of impairment/disability primarily looked ahead—to changing material circumstances for disabled people in the present and future. However, in recognition that perceptions of the past shape present action, it also influenced historical work.
Besides war (which often goes hand-in-hand with epidemic disease) and work, diseases have been the primary producers of disabled people (Kudlick 2014; Rembis 2019). Yet, disability history and the history of infectious disease and epidemics are typically siloed in separate fields. Historians Catherine Kudlick (2013, 2018) and Beth Linker (2013) have called for disability to be used not only as a topic for study but as a tool of analysis. Rather than epidemic mortality, Kudlick has argued for a focus on survivors of infectious diseases, such as smallpox, as a way not only to expand understandings of epidemics in history but also to bring disability history and medical history together. Survivors, rather than death tolls, are placed at the center of analysis. Epidemics have “a hidden history” of disability and survival, and examining this hidden history provokes questions about taken-for-granted ideas regarding personal, social, and political reactions and responses to both epidemic disease and disability (Kudlick 2014:197). Kudlick (2013) points to polio as the best example of existing work that brings together medical and disability history—though still with much scope for more.
Taking inspiration from and building on this work by historians, we envision similar developments in bioarchaeology, bringing together the paleopathology of infectious disease and the emerging (bio)archaeology of disability to better understand the impact of epidemics. Bioarchaeology can play an important role in locating impairment and interpreting societal reactions to such bodily differences and, as far as possible, the lived experience of disabled people (Rembis 2019). Authors such as Buckingham (2011) and Southwell-Wright (2013) have made the point that much of historical research relies upon, or predominantly represents, elite views and not the full spectrum of society. Additionally, marginalized groups are often underrepresented in quantitative historical data. Bioarchaeologists work with samples that often reach beyond the elite and therefore may better characterize the experiences of average and marginalized bodies. In the following section, we discuss the current state of bioarchaeological research on impairment and disability, with attention to its relationship with infectious disease.
Disability in Bioarchaeology
Early palaeopathological and bioarchaeological contributions in this area often showed interest in understanding an individual’s suffering or experience of disability (e.g., Brothwell 1961). In some of these early cases, authors were quite creative in presenting interpretations of skeletal material that today might seem baseless (e.g., some narrative work by Calvin Wells, as described by Waldron 2014). Tendencies to allude to the past feelings of individuals with impairments, and sometimes their caregivers, eventually inspired Dettwyler’s (1991) critique, “Can palaeopathology provide evidence for ‘compassion’?” While this work does articulate with concepts of impairment and disability, Dettwyler’s (1991) primary argument is against the unjustified interpretations of community motivations and compassion, as well as of the quality of life of impaired individuals in the past. This stern warning was likely warranted but unfortunately impeded much of the bioarchaeological commentary on disability for many years.
It took some time following Dettwyler’s (1991) publication, but near the end of the decade, volumes began to emerge that tackled themes related to identity, disability, and archaeology in new ways (Finlay 1999; Hubert 2000). These volumes integrated contributions from scholars and disability specialists in diverse fields, from anthropology to law to psychiatry. In one of these archaeologically focused collections, Cross (1999:24), a disability scholar, explains disability politics and adopts a social model perspective to remind readers of terminological differences and, very importantly, that “archaeologists dig up impairment, not disability.” Roberts (1999, 2000) also argues the importance of contextualizing disability, reminding readers that disability is something social and that its meaning and experience may differ. These socially informed perspectives were often published alongside medically oriented contributions that focused on interpreting “disadvantage” from skeletal evidence for disease and deformity and served to remind readers of the archaeological invisibility of people with impairments (Waldron 2000). A dichotomy in approaches did not go unnoticed at this stage, and prominent disability studies scholar Tom Shakespeare (1999:100) warned (bio)archaeologists to not be reductionists who confuse “the biological evidence with the social experience.” Shakespeare (1999) also observed a lack of consistency with our terminology at this stage, placing bioarchaeologists out of step with the broader disability studies context.
Discussion surrounding the interpretation of disability from skeletal and archaeological data slowed again at this point. Some publications in the 1990s investigated impairment, such as Knüsel et al. (1992) and Hawkey (1998). However, for the most part, these publications examined physical function as it is preserved in the skeleton, rather than engaging directly with disability studies literature, theories, and terminology. In the later 2000s and early 2010s, we saw bioarchaeologists revive this discourse, alongside advancements in how we conceptualize bodies (e.g., Sofaer 2006). Knudson and Stojanowski (2008), for example, engaged with the social model of disability and reflected on disability as an aspect of individual social identity that might be elucidated from funerary contexts and skeletal remains. We then saw inquiry into disability in archaeology pickup, with contributions critiquing the under-theorization of this area of study within anthropology and reinvigorating dialogue with a greater connection with the disability studies literature (e.g., Battles 2011; Southwell-Wright 2013).
In the mid-2010s, a new angle to looking at human experiences of impairments and possible disabilities was introduced by Lorna Tilley (2012) in the form of the bioarchaeology of care. The bioarchaeology of care model has since been thoroughly explored in various volumes and studies (e.g., Tilley 2015; Tilley and Cameron 2014; Tilley and Schrenk 2017). Despite earlier calls for more direct engagement with disability studies literature when looking at difference in the past, Tilley’s work continues to take a more medicalized approach, adopting definitions and conceptualizations of disability as outlined by the World Health Organization (Tilley and Schrenk 2017:16). The research rigor that is encouraged by the use of the bioarchaeology of care framework is admirable and has resulted in many published case studies by researchers wishing to better understand the experiences of past people (e.g., Málaga and Makowski 2019; Solari et al. 2020; Tornberg and Jacobsson 2018; and many more). For example, Tilley and Nystrom (2019) applied this model in their analysis of the mummified remains of a Nasca child from Peru (ca. 700 A.D.) with evidence for tuberculosis. The insights drawn from this case allow researchers to interpret that the Nasca people “cherished their children,” giving greater insight into this culture’s daily life (Tilley and Nystrom 2019:79). While some of this wealth of care-related literature reaches into individual, social, and cultural perceptions of impairment as it relates to care provision, it does not explicitly engage with the realm of critical disability studies as advocated in the 1990s.
Alongside the bioarchaeology of care, we have seen the emergence of additional discussions of diverse human experiences and frameworks for the bioarchaeology of personhood (Boutin 2016) and the bioarchaeology of impairment and disability (Byrnes and Muller 2017; Matczak et al. 2019). While some volumes (e.g., Byrnes and Muller 2017) integrate voices from critical disability studies such as Shuttleworth and Meekosha (2017), in practice, much of the bioarchaeological work remains grounded in more medically oriented models of disability. Like the bioarchaeology of care, this developing bioarchaeology of impairment and disability predominantly relies on the frameworks and definitions by the World Health Organization that are familiar to modern clinicians. Alternatives, such as the bioarchaeology of personhood proposed by Boutin (2016), have more social-model foundations; they argue once again that disability has been under-theorized by bioarchaeologists and indicate that possibilities to better interact with diverse public audiences must be promoted. Approaches that engage more with embodiment and intersectional identities (Gowland 2017; Schrader and Torres-Rouff 2020) also have considerable potential in their recognition and engagement with critical and social disability theories.
Although more socially informed models exist in bioarchaeology, they have not gained as much traction as the medically driven frameworks. It is difficult to explain why this might be, as the critical disability engagement with bioarchaeology has been calling out for more theoretical nuance for the past 25 years. Perhaps our persistent adoption of the medical approach is a tactic that permits bioarchaeologists to still firmly situate their evidence for disability within the analysis of the human body itself, through the skeletal remains. However, if we continue to choose this route, we must remember Shakespeare’s (1999:100) critique and be absolutely certain we are not confusing “the biological evidence with the social experience.” Bioarchaeology has the potential to greatly broaden the scope of what we can learn about experiences of epidemic survivorship and disability in the past. By continuing to develop our discipline, as well as how we view and interpret past lives and experiences, we can work to better represent the diversity in humans as well as the repercussions of epidemic disease.
Envisioning a Survivor Lens Approach
In this section, we explore how approaching archaeological assemblages using a survivor lens will improve our understanding of the consequences and human experiences of infectious disease. It is important to note that this new theoretical nuance in epidemic interpretations must be adapted and flexibly applied depending on the context; different diseases will require their own unique methodological techniques and contextualized interpretations using this approach. Due to considerable variation in diseases, contexts, and possible methods of investigation, we are not able to prescribe a specific “how-to” for identifying and interpreting survivors in bioarchaeology; there are simply too many factors that are unique in each situation. Instead, to demonstrate the importance of our aims, we use poliomyelitis and other infectious disease examples to discuss how a survivor lens can illuminate survivors’ individual, social, and cultural experiences and contributions and therefore extend bioarchaeological interpretations.
Poliomyelitis is a disease caused by infection with one of the smallest known viruses, an enterovirus in the Picornaviridae family of RNA viruses, with three serotypes that vary in neurovirulence. It is an enteric infection spread through the fecal–oral route (contaminated water or food or person-to-person via contaminated hands) or by droplets or aerosols (person-to-person). The poliovirus spreads from the throat or intestines to the lymph nodes and then to the bloodstream. From there, it may enter the central nervous system, where it damages motor neurons, causing paralysis and other complications (Smallman-Raynor et al. 2006). Symptoms of polio infection can vary from sore throat, headache, and other signs of influenza-like illness to severe and potentially fatal paralysis and encephalitis.
Polio likely affected some individuals in the past. However, reported cases are relatively rare in the archaeological literature and in all instances represent case studies of individuals with some degree of paralysis (possible archaeological cases of polio are summarized by Novak et al. 2014 and Berner et al. 2021). Poliomyelitis can be remarkably debilitating but results in relatively low mortality in the regions where it is endemic. With the wealth of modern clinical and archival literature available on polio and survivors’ experiences, as well as its propensity to leave identifiable skeletal indicators in some infected individuals, there is significant scope for investigating polio’s past epidemic legacies. Moreover, poliomyelitis serves as a perfect example to demonstrate the importance of looking beyond epidemic-related deaths and pivoting our perspectives to more fully consider an epidemic’s survivors while keeping a familiar touchstone of identifiable skeletal lesions upon which palaeopathologists typically ground their interpretations. In the following sections, we consider three questions: If epidemics were as common in the more distant past as they were in recent history, where are all the survivors in archaeological contexts? What can infectious disease survivors tell us? And how does taking a survivor lens to view the (pre)history of epidemic disease change our perspective? These scaffolded questions move through multiple levels of analysis: from the individual body, to the social and interpersonal, to the drivers of cultural change.
Where are all the survivors? Individuals and bodies
Traditional palaeopathology often relies on the observation of skeletal lesions (e.g., lytic and blastic bone responses). However, individual infections and their sequelae may not result in osteological changes or be identifiable via biochemical techniques. Bioarchaeologists are accustomed to working within these limitations to investigate conditions that only manifest skeletally in a subset of all those infected. For example, tuberculosis affects the skeleton in only 3% to 5% of cases (Roberts and Buikstra 2019). Table 1 provides examples of a variety of infectious diseases that are often associated with long-term sequelae; some leave skeletally observable indicators, but many may leave no trace (see also Valerio et al. 2020:Table 2 for examples of epidemic diseases with known neurological complications). Because there will almost always be a subset of individuals who live through an infectious disease but do not manifest skeletal lesions, bioarchaeologists must still remember that these “invisibly” impaired individuals exist within the assemblages we are investigating. Palaeopathologists and bioarchaeologists are already experienced with considering such cases as a subsample of a wider survivor population and should therefore be well positioned to take on a survivor lens that relies on careful extrapolation of diseases and their sequelae from the individual to group levels.
By considering the long-term consequences of polio more closely, we can explore the challenges associated with accounting for survivors in archaeological contexts. There are three clinically recognized forms of poliomyelitis: abortive (minor illness only), nonparalytic (major illness without paralysis), and paralytic (major illness with subsequent paralysis). Paralytic polio is one of the most recognizable expressions of this disease and typically results in acute flaccid paralysis (i.e., muscle weakness or paralysis with sudden onset) of one or more limbs (Smallman-Raynor et al. 2006). However, the vast majority of infections are asymptomatic or with such mild symptoms that the infection goes unnoticed; between 4% and 8% are the abortive form and only 1% to 2% become major illnesses (e.g., paralytic) (Smallman-Raynor et al. 2006).
Table 1. Selected Infectious Diseases and Associated Sequelae.
|
Disease |
Pathogen |
Potential for Reactivation?1 |
Sequelae (General Synopsis with Selected Examples)2 |
Sources |
||||
|
Chickenpox |
Varicella-zoster virus (VZV) |
Yes; reactivation may be acute second episode or become chronic |
Reactivation of VZV as shingles can lead to a chronic syndrome called postherpetic neuralgia and can include encephalitis, vision loss, facial palsy (Ramsay-Hunt syndrome), and chronic paralysis of an extremity. |
Hayashi et al. (2009) |
||||
|
Poliomyelitis |
Poliovirus |
No |
The main characteristic of polio is acute flaccid paralysis affecting one or more limbs. Limb shortening may occur if the infection occurs before skeletal maturity, and muscle impairment or paralysis and compensatory biomechanical use may cause other osseous changes. For example, scoliosis may develop due to asymmetrical trunk paralysis. Post-polio syndrome occurs in a large proportion of paralytic polio survivors and is characterized by renewed, progressive muscle weakness; muscle and joint pain; and fatigue decades after original recovery. |
Grauer and Roberts (2019); Smallman- Raynor et al. (2006) |
||||
|
Smallpox |
Orthopoxvirus variola, aka variola virus. Two variants (major and minor) |
No |
Smallpox infection often leads to scarring, sometimes severe enough to prevent eyes from opening, resulting in impaired vision or blindness. Ocular complications are another potential cause of blindness. Infection of the bones and joints (osteomyelitis variolosa) can cause bone lesions, deformity, joint fusion, and lasting joint pain. The elbows are particularly likely to be affected. |
Darton et al. (2013); Grauer and Roberts (2019) |
||||
|
Syphilis |
Treponema pallidum pallidum |
Yes |
While this disease may not initially easily fit the “survivor” model proposed in this article, syphilis is argued to have appeared in a more virulent epidemic form in certain times and contexts, such as in late fifteenth/early sixteenth-century Europe and in nineteenth-century Australia as the disease was introduced to the Aboriginal population by European colonists. As such, in some contexts, syphilis can be viewed as an epidemic condition using a survivor lens. T. pallidum bacteria infect the skin and mucous membranes, with progressive stages of the disease divided into primary, secondary, and tertiary forms (with latent asymptomatic periods). Long-term infection can lead to lesions and changes in various bodily systems, particularly the skin and the cardiovascular and musculoskeletal systems, including aortitis (the most common cause of death from syphilis), gummatous osteomyelitis, periostitis of the long bones and cranium, and pseudo-rheumatism. Early congenital syphilis (birth–2 years) can include hydrocephalus and osteochondritis with pseudoparalysis of the limbs. Late congenital syphilis (>2 years of age) can include gummatous lesions (leading to saber shins and bossing of the frontal and parietal bones) and maldevelopment of the maxilla and dentition. Deafness and blindness are also potential sequelae. |
de Melo et al. (2010); Dowling (1997); Fratamico et al. (2009); Klausner and Freeman (2009); Tesini (2020) |
||||
|
Tuberculosis (TB) |
Mycobacterium tuberculosis |
Yes |
Tuberculosis infection is divided into three stages: primary infection, latent TB, and chronic active TB. If the initial primary infection becomes disseminated throughout the body, complications such as tuberculous meningitis (which occurs most often in young children or immunosuppressed individuals) may develop. In chronic active TB, as the disease progresses, symptoms such as fevers and anorexia develop, and in terms of extrapulmonary TB, lesions and abscesses can occur in multiple sites or tissues. TB can affect bone in approximately 3% to 5% of cases. Foci are most commonly found in the vertebrae (known as Pott’s disease, with potential for spinal cord compression; Pott’s paraplegia; and kyphosis due to vertebral collapse) and joints, such as the hip and knee, which can lead to dislocation, ankylosis, and/or arthritis. |
Roberts and Buikstra (2019); Greenstein et al. (2009) |
1The diseases and pathogens listed are those with an initial acute infection phase after exposure, after which the pathogen may be either cleared from the body or persist in a latent phase with the potential for later reactivation. In this article, a “survivor” refers to someone who did not die in the acute infection phase.
2We have included a selection of sequelae with an emphasis on those potentially observable bioachaeologically, particularly on skeletal remains. We have also included some conditions less likely to be visible bioarchaeologically to give a broader representation of the possible impairments. The sequelae listed here do not represent all potential sequelae of each disease.
Modern bioarchaeological studies have discussed possible cases of the paralytic form of poliomyelitis in archaeological skeletons based on the observation of skeletal traits indicative of the associated disuse and altered function. The most commonly reported skeletal changes include shortened limbs, bone atrophy, and torsion and abnormal curvature of long bones (Castells Navarro et al. 2017; Ciesielska and Stark 2020; Gładykowska‐Rzeczycka and Śmiszkiewicz‐Skwarska 1998; Kozlowski and Piontek 2000; László 2017; Novak et al. 2014; Thompson 2014). Scoliosis and skeletal evidence of clubfoot are also regularly mentioned (e.g., Castells Navarro et al. 2017; Winkler and Grosschmidt 1988). Although there are some distinguishing features of paralytic polio, poliomyelitis has only rarely been diagnosed in archaeological human remains despite being potentially common in the past. The apparent “rarity” of polio is perhaps not surprising given that only a small minority of poliovirus infections tend to develop into major illnesses with long-term sequelae. However, even one or two in 100 infections developing into paralytic cases adds up to a large number of potentially visible polio survivors. This prevailing perception of polio as a “rare” disease is addressed by Berner et al. (2021), who argue for the use of a number of specific geographic, environmental, demographic, and cultural variables in the systematic analysis of ancient cemeteries. They offer a specific methodological approach to the diagnosis of paralytic poliomyelitis in survivors and suggest development of a measure of this “rarity” for this and other diseases yielding a ratio of prevalence with a community (Berner et al. 2021). We encourage readers interested in exploring specific methods for investigating survivors to consider Berner et al.’s (2021) suggested approaches.
Recognizing polio as a “common” rather than a “rare” disease does not mean assuming it was evenly distributed across populations. Urban, rural, and remote contexts would be differentially affected; the virus could only be established (endemic) in large urban settlements of 250,000 people or more (the critical community size for poliovirus; Eichner et al. 1994). Smallman-Raynor et al. (2006) classify polio as being in this endemic phase in large populations prior to (ca.) 1880 A.D. In endemic polio contexts, most manifestations of the disease would be abortive (i.e., minor) and occur in infants—who, once they had contracted polio once in their life, would develop immunity and be unlikely to contract a more severe form later. In contrast, populations who had never before encountered polio would be more likely to have higher mortality and larger groups of people affected with more severe disease sequelae (Paul 1971). In any population where the poliovirus was new—and people had no immunity from prior exposures—it is a logical possibility that a substantial outbreak would have occurred upon that population encountering the virus for the first time. For example, the 1947–1948 polio epidemic in the Nicobar Islands appears to have been largely a “virgin soil” epidemic, with approximately 10% of the population developing symptoms of paralytic polio and causing 280 deaths; in one village, 15.8% developed paralytic polio, and 3.9% of the population died (Moses 1948; Smallman-Raynor et al. 2006:422–424). A 1949 outbreak in Chesterfield Inlet, Nunavut, Canada, left over 14% of its Inuit population of 275 people with paralysis and caused 14 deaths—a mortality rate of over 5% (Adamson et al. 1949). Total morbidity for the outbreak (those showing any symptoms of the infection) was estimated at 50% or more (Adamson et al. 1949).
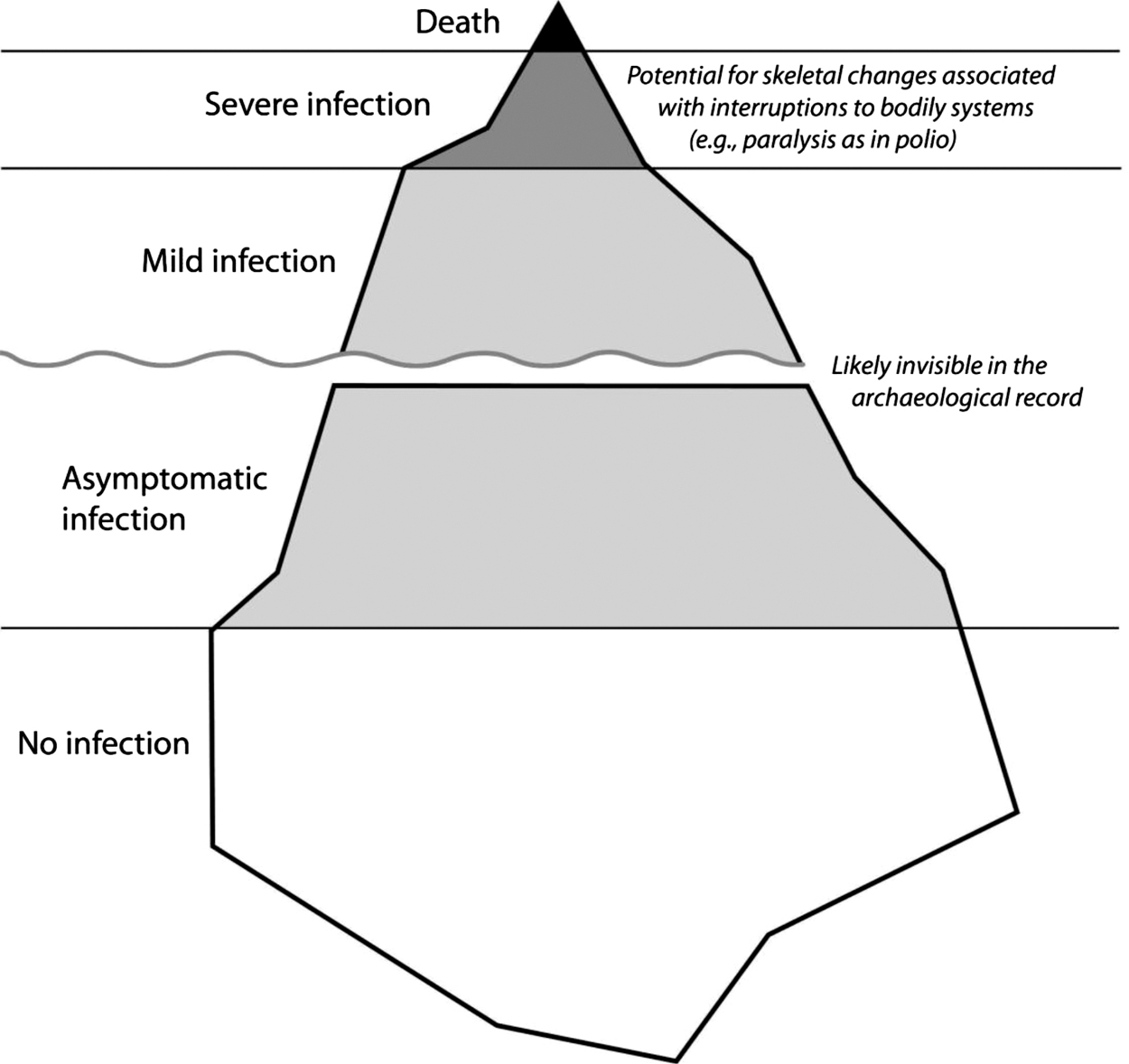
Polio here nicely demonstrates the “iceberg concept of infection,” described by Evans (1984) as referring to a biological gradient of host response to a pathogen. Some pathogens, such as the viruses that cause rabies and measles, cause clinically apparent illness in all or nearly all infections of human hosts. In others (such as poliovirus), clinical illness comprises only a small proportion of the host response pattern, with asymptomatic or unrecognized infections making up a larger share (Evans 1984). We have adapted Evans’s original analogy and diagram to represent the implications of this gradient for the visibility of sequelae in the archaeological record, visually indicating relative proportions of individuals who may show disease sequelae in osteological contexts versus those who likely will not (Fig. 1).
Figure 1. Diagram illustrating the “iceberg concept of infection” and its implications for visibility of sequelae in the archaeological record. Adapted from Evans (1984:Figure 2, 20).
Bioarchaeology (in terms of analysis of skeletal remains in their archaeological context) may be one of the few options available for learning more about the history and origins of polio. Genomic investigations are not promising options to advance our ability to identify polio survivors; as a tiny RNA virus that rapidly accumulates nucleotide substitutions, poliovirus does not survive for ancient genomics analysis and also does not lend itself to phylogenetic reconstruction beyond only the very recent past (i.e., past several decades) (Jorba et al. 2008; Kuge et al. 1989; Rico-Hesse et al. 1987). In summary, it is nearly impossible to see polio epidemic deaths that happen in the acute stage bioarchaeologically—no ancient RNA, no signs on the body/skeleton, and unlikely mass mortality. This leaves the bodies of the survivors (i.e., those with the longer-lasting sequelae such as paralysis) as the only bioarchaeological evidence—a small but visible portion of the “infection iceberg” in which deaths represent only the very tip (see Fig. 1). Polio, therefore, forces us to look at the survivors, not the fatalities—an important lesson that can be extended to other infectious diseases regardless of how they manifest skeletally.
Based on the iceberg model of infection, as long as even one skeletal case of paralytic polio is identified, it can be inferred that other instances of the disease were also present in the population, albeit perhaps in other forms (e.g., abortive, nonparalytic). Although the exact infection rates may remain unknown, the link between skeletally visible and invisible cases is clear. Blanket interpretations, however, about survivors and rates of survivors are typically not possible due to contextual variability in infection rates (e.g., urban versus rural) and differences in the rate that sequelae manifest. As such, it continues to be vital that bioarchaeologists and palaeopathologists situate their interpretations carefully within each context and remember that the individuals with lesions represent only a subset of the whole survivor cohort.
What can survivors tell us? Social landscapes and behaviors
Building on an understanding of the presence of visible and invisible survivors in the archaeological record (see previous section and Fig. 1), it is next necessary to explore how individuals and their bodies interact with the existing social landscape. This section explores the “social” impacts on and experiences of survivors through health care practices, treatments, and functional outcomes, as well as stigma enacted by other members of their communities. While discussing the social impacts on individuals, we also revisit (social model) distinctions between impairment and disability and consider the role these perceptions of difference may play in survivors’ experiences. By applying a survivor lens while considering the aftermath of epidemics, this section shows how we might move beyond individual bodies to better understand the social circumstances within which they lived and how these circumstances may have shaped survivors’ lives.
Treatment is often a necessary intervention to ensure survival and achieve outcomes that are perceived as optimal. Although lives, functional abilities, and/or appearances may have been preserved, these same treatment interventions can also sometimes cause poor long-term outcomes in survivors. Immobilization and bedrest are examples of treatments that may help individual health and mobility outcomes but come with potential detrimental trade-offs. Immobilization was a common practice in twentieth-century polio epidemics, with the goal of preventing skeletal deformities (Ross 1993); however, it also contributed to muscle atrophy and reduced joint flexibility (Altenbaugh 2015). In tuberculosis sanitoria, bedrest was a common treatment in order to “immobilize the lungs” (Coryllos 1933). In both these cases, extended periods of immobility would affect all bodily systems and could contribute to an individual’s overall “frailty,” leading to increased fracture risks due to reduced bone mass and central nervous system changes creating reductions in balance, as well as respiratory and cardiac complications (Dittmer and Teasell 1993; Teasell and Dittmer 1993). Bioarchaeological studies such as those by Sparacello et al. (2016) and Mansukoski and Sparacello (2018) underscore these periods of reduced mobility in the past and report skeletal evidence for growth interruptions and increased gracility in individuals associated with responses to or risks for chronic tuberculosis infection. Thus, the skeletal material (and the impairment experienced in life) reflects not only disease processes but also ideas about proper treatment and intervention as well as ideal outcomes in terms of function and aesthetics.
In terms of their experiences as survivors, people who have had polio, especially those with severe paralysis, are also subject to increased mortality in the long term (Nielsen et al. 2003). Among other risks, potentially fatal complications such as pneumonia may develop over time. Furthermore, decades after recovery from the initial infection, polio survivors can develop “post-polio syndrome,” characterized by symptoms including muscle weakness and fatigue. The cause is believed to be a failure of the motor neurons that compensated for the damage from the original infection (Jubelt and Agre 2000). Thus, even after a period of recovery and stability, polio survivors can still experience increasing impairment and disability. Estimates of the proportion of survivors who go on to develop post-polio syndrome range from 28.5% to 64%, with those who had more severe acute infections followed by greater functional recovery apparently at higher risk (Jubelt and Agre 2000; Ramlow et al. 1992; Windebank et al. 1991).
Bioarchaeologists who have considered polio as a possible cause for the skeletal changes they observed have focused on a range of interpretive outcomes. Early work by Mitchell (1900) was concerned with morphology and patterning of the asymmetry but still considered the ways that the affected individual may have compensated for their different leg lengths through the use of high-soled sandals and balancing staves. This interest in individuals’ mobility carries on in modern studies, where researchers use similar observations and measurements to comment on the functional consequences of paralytic polio (Novak et al. 2014). Other scholars strive to interpret the experiences of individuals with neuromuscular conditions using frameworks such as the bioarchaeology of care. Although polio was listed as just one of many possibilities, Schrenk and Martin (2017) adopt this approach with the case of an 18-year-old female from the Bronze Age United Arab Emirates in order to understand her experience of care as well as social and community relationships. They suggest that this individual likely needed some care provision that was provided predominantly by her close contacts but was also able to be somewhat self-sufficient with her upper body as long as materials were within reach (Schrenk and Martin 2017). A more quantitative approach is proposed by Stodder (2017), who adopts the World Health Organization’s Global Burden of Disease (GBD) project model (and its associated metrics of disability weights and years lived with disability) to focus on morbidity over mortality and better deal with conditions that do not fit easily into specific etiological frameworks. One of the categories in the GBD model, “Impairment (hip, leg, foot),” was originally designed for polio sequelae but later expanded to include non-polio causation (Stodder 2017:note on Table 10.1, 188). The advantage of the GBD approach, she says, is that it can reveal things about a population’s health that are masked in demographic statistics, such as in life tables (Stodder 2017).
We have established that following epidemics, there is often a subset of the population that experiences long-term and potentially impairing consequences. These impairments can be invisible and private, but they can also be recognized within communities and among individuals. In some cases, this visibility results in judgment and prejudice against those individuals because they have been (or continue to be) affected by a disease, which may carry a stigma. This stigmatization has the potential to alienate individuals and groups of individuals in a society and fuel health inequalities (Hatzenbuehler et al. 2013; James et al. 2020). It can also result in additional (negative) outcomes related to the embodied experiences of stigma. For example, stress is one pathway through which stigma can become embodied. The physiological stress response elicited by exposure to stigma can slow recovery and increase a person’s chances of developing complications such as secondary or additional infections, while psychosocial stress can have serious mental health impacts (Brewis et al. 2020). Stigma associated with an infectious disease and/or its sequelae can also reinforce existing stereotypes and heighten discrimination when concentrated in already marginalized groups; such intersectional stigma can lead to the compounding of suffering (Brewis et al. 2020; for discussion of intersectional analysis in bioarchaeology, see Mant et al. 2021 and Yaussy 2019). Furthermore, visible and impairing sequelae following infection with a contagious disease can also increase suffering by bringing discrimination and the stigma of disability and difference into the mix.
Stigma around polio in the twentieth century could manifest in different ways, such as the perception of polio survivors as dangerous spreaders of contagion even long after recovery. For example, one polio survivor recalls, “Years after I had polio, when adults saw me coming they would say out loud to their children to stay away from me because they could ‘catch it’” (Bruno 2002:83). Polio survivors were also subject to overt and more generalized prejudice associated with their new disability status. Bruno remembers another incident in which a stranger on the street one day stopped him and declared, “You cripples shouldn’t be allowed in public!” (Bruno 2002:83). It is clear that polio survivors experienced stigma and social exclusion in the historical past. These examples, combined with other historic and archaeological examples of stigma associated with infectious diseases (e.g., leprosy), support the idea that people with infectious disease sequelae in other contexts may have been treated differently following infection.
Investigations of archaeological difference have the potential to yield enormous insight into the social circumstances existing after an epidemic disease (e.g., Hubert 2000). By using existing bioarchaeological theories and methods (embodiment, bioarchaeology of personhood, bioarchaeology of care) strongly grounded in a contextual understanding of the region and time, survivors can be remembered and situated in their social landscapes to better infer their specific experiences and how they were shaped by community attitudes. Work on leprosy and leprosaria already deals with many of these questions (e.g., Roberts 2011, 2020; Robbins Schug 2016), and these approaches may be useful as we continue to consider survivors of other epidemic infectious diseases and the social and embodied repercussions they encountered.
While stigma is frequently associated with infectious diseases and their sequelae, it is imperative that bioarchaeologists always ground interpretations of stigma experienced by survivors in appropriate contextual data. We must not apply our modern understanding of disease perceptions to the past, as they very well may have differed. This is nicely demonstrated by Robbins Schug’s (2016) investigation of the evolution of stigma against people with leprosy in South Asia. Using both mortuary evidence and textual analysis, Robbins Schug situates shifts in the disease experience of leprosy within changes in climate, politics, economy, and society, particularly major fluctuations in urbanism over millennia. She finds that at some points in time, leprosy was much less stigmatized by community members than at other times. Her findings demonstrate a clear destabilization of the assumption that stigmatization and othering of people with leprosy is natural and universal (Robbins Schug 2016). In other words, the presence of disease or related sequelae alone does not predict the occurrence of stigma or preface the development of changes in social behaviors associated with treatment of individuals with disease repercussions.
Robbins Schug’s (2016) research provides a valuable example of bioarchaeological work that de-naturalizes the link between the medical (disease, impairment) and the social (disability). The primary point of the social model is not that there is no relationship at all between the two but rather that impairment does not have to lead to disability. Taking a survivor lens approach, embedded with understanding of the socially nuanced differences between impairment and disability, will tell us much about survivor experiences of not only their bodies but also the broader social landscape in which they lived, including the nature and impacts of treatment and stigmatization.
How does taking a survivor lens change our perspective? Cultural insights and developments
This focus on survivors—not those that simply made it through the epidemic event, but those whose bodies were permanently marked by the disease (visibly or not)—gives us a different perspective on the disease and its impact, on both the pathogen as it moved through human populations and on how populations and societies were changed by its effects. People with bodies sharing the same “designations of deviance” can find themselves clustered together in certain settings (e.g., institutions) and/or discover that their critical mass allows for effective collective social and political action (Snyder and Mitchell 2006:185). We know, for example, from histories of the past century that the emergence of large cohorts of wounded soldiers and polio survivors led to major medical, political, and social changes, from advances in orthopedics to the disability rights and disabled consumer movements and their wide impact (see, for example, Kaufert and Kaufert 1984; Liebenberg 1994). Despite such progress, many of our assumptions and interpretations, driven by modern cultural perspectives, are still ableist in nature. Ableism is a set of ideas, values, and practices that hold able-bodiedness as the standard of normalcy, desirability, and productivity and accordingly marginalize, oppress, and render “invisible” those who deviate from that standard (Chouinard 1997; Wolbring 2008). Particular configurations of ableism today can shape our approach to the past. In order to challenge culturally ingrained preconceptions, this section works to illuminate how contributions and innovations led by survivors helped to drive meaningful cultural changes in the perception of, and attitudes about and toward, disabled people.
The large and recurring polio epidemics of the early twentieth century, combined with standard immobilization treatments, resulted in an increasing need for polio aftercare. At the same time, the First World War also created a similar demand for treatment of wounded, disabled soldiers. Both of these events, and particularly their historical confluence, are credited with laying the groundwork for modern physical therapy (Altenbaugh 2015) as well as modern orthopedics (see Battles 2019; Ross 1993). Orthopedic surgeons and rehabilitative therapists often took treatment techniques originally developed with one group and applied them for the other. For example, once the influx of wounded troops to New Zealand’s military hospitals waned, the hospitals transitioned to civilian use, and the orthopedic expertise of military medical staff was applied to the treatment of polio survivors (Battles 2019). In the same vein, physical therapy techniques developed in the care of polio survivors after the 1916 epidemic in New Zealand were seen as potentially useful for the care of the war-wounded (see Battles 2019). Perhaps unsurprisingly, these two groups (polio survivors and wounded soldiers) sometimes found themselves co-resident in the same facilities, with significant impact on their experiences of rehabilitation (see, for example, Battles 2019 and Ross 1993 in New Zealand and Koven 1994 in Great Britain).
While these rehabilitative institutions and their associated treatments typically operated with the goal of shaping bodies to fit back into an able-bodied normative world, at the same time, there is an extensive literature on how polio survivors shaped their societies and cultures in the twentieth century. The impact of polio on culture is particularly evident in countries where waves of polio epidemics led to the emergence of institutional patient cultures and community formation among disabled polio survivors (see Altenbaugh 2015; Gallagher 1998). The form these communities and impacts took depended on local and, particularly in the twentieth century, national contexts. In Cold War Hungary, for example, the ideas and values of modernity, industry, and production shaped the rehabilitative treatment of polio survivors, with training for specific trades (Vargha 2018b). Similar to work offered in other institutional rehabilitative settings, these trades consisted of watch repair and shoemaking for boys and men, and work in the prosthetics factory for girls and women (Vargha 2018b). Furthermore, Vargha (2018a) describes the formation of a civil society in the late 1970s by Hungarian polio survivors who drew on their institutional networks developed during their long periods in the hospital. Their aim was to achieve disabled people’s full participation in society and as such organized themselves to provide for each other and to call upon the state to fulfill its responsibilities toward them (Vargha 2018a). Finding their institutional occupational training restricted their options for education and work, Hungary’s National Association of Disabled Societies established a packaging company that provided its members with work options (Vargha 2018a). To organize such a society that was neither directly opposed to the government nor co-opted by it was a remarkable thing in the midst of a communist state (Vargha 2018a). While their placement within institutions and the emphasis on normative bodies are less than ideal, these social circumstances within which survivors lived provided an opportunity for cultural reformations found through the development of disability-led communities.
One of the most famous polio survivors was former U.S. president Franklin D. Roosevelt (FDR). FDR contracted polio in 1921 when he was 39 years old, which developed into the paralytic form. Although he made efforts to downplay any disability during his time in office, he was instrumental in establishing the Warm Springs Institute, a comprehensive rehabilitation center initially focused on post-polio recovery in all its physical, psychological, and social dimensions (Holland 2006) but which today includes rehabilitation for other spinal cord and stroke-related conditions. Although FDR was just one survivor, the innovative nature of the Warm Springs Institute created an important community for many disease (polio) survivors; a number of future disability rights activists (e.g., Hugh Gallagher, discussed further below) spent time there (see Patterson 2012). Holland (2006) describes Warm Springs in the 1920s to 1940s as an enclave where the stigma of disability was not only transcended but the medical model of disability itself was challenged. Quality of life, rather than a “cure,” was the focus (Holland 2006). Furthermore, the physical environment of Warm Springs was designed to be fully accessible—one of the few outdoor facilities to do so at the time (Holland 2006).
This rehabilitation center, initiated by a disabled infectious disease survivor and hosting a similar survivor community, with disabled people in leadership positions as staff and board members, is argued to be the precursor to the disability rights, universal design, and independent living movements (Holland 2006). Warm Springs not only foreshadowed these later movements but directly influenced them; for example, Fred Fay, who spent two years at Warm Springs, established the Boston Center for Independent Living in 1974 (Holland 2006). The independent living movement argues for reinvention of medical model–style rehabilitation and education programs (Holland 2006), with disabled people, rather than medical professionals, in control. It drew inspiration from other movements, including the civil rights movement of the 1950s to 1960s, and has been instrumental in changing the way that disabled people live day-to-day. At the same time, the operation of Warm Springs as a white-only facility in the American South fostering white leadership also influenced the shape of the American disability rights movement (i.e., problematically, as a predominantly white-led initiative) (Patterson 2012). Due to these facilities established by a survivor who created communities for survivors, we can clearly see cultural changes in ways of living and social perception that affected not only the survivors, but also their families, community members, and broader society.
As with the First World War, the aftermath of the Second World War combined with polio epidemics amid the postwar baby boom spurred political and public support in the United States to fund rehabilitation and develop new mobility aids (Altenbaugh 2015). This increase in war- and disease-related impairments also led to changes in architecture and design (e.g., single-level homes) and adapted vehicles (e.g., introduction of hand controls) (Altenbaugh 2015:191 citing Gallagher 1998; Buick Motor Division 1946). In the United States, activists such as Edward Roberts, Judy Heumann, Mary Lou Breslin, and Hugh Gregory Gallagher—all polio survivors who used wheelchairs—had substantial impacts on changing policies and regulations for accessibility, some of which led to major changes in built environments. For example, Roberts and other members of an activist group of disabled students at the University of California at Berkeley, known as the “Rolling Quads,” campaigned for better physical community access (e.g., curb cuts in sidewalks to facilitate wheelchair mobility) and lobbied the university to establish a Physically Disabled Students Program, for which they obtained a federal grant to fund staffing, wheelchair repairs, and other access needs (Danforth 2018; Patterson 2012). The Rolling Quads emerged from a community of students who lived on the third floor of a campus hospital, which, unlike the dormitories, was wheelchair accessible and had room for Roberts’s “iron lung” respirator (Patterson 2012). From this beginning, in 1972, two of the Rolling Quads established the first Center for Independent Living, which became a model for hundreds of similar centers around the United States (Danforth 2018; Patterson 2012).
These actions at Berkeley launched the independent living movement (see above) and attracted disability activists from across the country, including Judy Heumann (Patterson 2012), while influencing others such as Mary Lou Breslin (already at Berkeley) to become active in disability rights activism (Wolfe 2012). While at university in New York, Heumann had advocated for ramp access to her classroom; in 1970, along with others (some of whom she had met as a child at Camp Jened, a camp for disabled children), she founded the civil rights organization Disabled in Action. Breslin cofounded the Disability Rights Education and Defense Fund, a leading national civil rights law and policy center, in 1979 (Wolfe 2012). Among Gallagher’s extensive contributions to disability rights in the United States (see his autobiography [Gallagher 1998], as well as discussion in Altenbaugh 2015), as a Senate staffer, he drafted the Federal Architectural Barriers Act of 1968, which required that all public buildings, or those in which physically impaired individuals might reside or work, financed with federal funds be designed and constructed in accordance with prescribed accessibility standards (Architectural Barriers Act 1968). Similarly in Hungary, polio survivors were instrumental in the establishment of the National Federation of Disabled Persons’ Associations (MEOSZ), the country’s largest nongovernmental organization for representing and advocating disability rights (Vargha 2018b). Polio survivors were thus at the center of twentieth-century changes to the built environment for physical accessibility and increased representation of disabled people during decision-making affecting them.
The previous examples provide valuable context to indicate that disabled people have been active in designing and driving changes in built environments; there is no reason to believe that their input and innovation were excluded in the past. Early on in archaeological investigations of disability, Cross (1999) proposed that archaeologists should be considering the landscapes and built environments in which individuals lived. Sneed (2020) approaches these questions through her investigation of ramps used in ancient Greek architecture, arguing for the potential influence of the presence of people with mobility impairments on architectural choices for public spaces (healing sanctuaries). There is still much room to investigate relationships between bodies and space in archaeological contexts, and as the historic examples demonstrate, we should remember that some design elements may indeed have been driven by the survivors themselves.
To operationalize the survivor lens, we must continue to practice good palaeopathology and bioarchaeology through multiple levels. Rather than prescribing a specific method or radically new approach that will necessarily differ based on context (see “Where are all the survivors? Individuals and bodies” section), the survivor lens represents a subtle theoretical shift that allows us to envision group-level experiences, such as the impact of a sudden cohort of disabled people in a community or society. As demonstrated here, the history of polio in the twentieth century demonstrates how diseases can become “imprinted on the bodies of survivors, societies and cultures” (Vargha 2018a:181). The ways polio survivors and others dealt with the consequences of polio infection brought about diverse impacts on society and culture, from changes in medical treatment and built environments to community formation spurring advocacy and activism that led to yet bigger changes on the national and international scale. This is a clear difference in focus from approaches such as the bioarchaeology of care. Not only is there an explicit emphasis on the group-level impact of the presence of a survivor cohort, but the survivor lens considers survivors to be potential drivers of innovation and change—including as active agents of that change. A survivor lens can thus help bioarchaeologists consider both the long-term impacts that epidemic survival has on individuals and their immediate relations, as well as in shaping societies.
Conclusion and Future Directions
In the COVID-19 pandemic thus far, as in the bioarchaeology of past pandemics, the focus of concern has largely been on deaths. COVID’s “long-haulers” remind us, however, that the effects of such outbreaks include long-term morbidity and disability for the survivors of infection—often in proportionately larger numbers than the death toll. Polio is an example of such a disease with sequelae that are potentially visible in the archaeological record, and it prompts us to think of the possibilities of approaching the study of past epidemics a bit differently. One potential source of guidance or inspiration we can look to is developments in the field of disability history, particularly Kudlick (2013, 2018) and Linker’s (2013) calls for bringing together usually “siloed” fields in considering the survivors of epidemic infections. Similarly, bioarchaeology of infectious disease and epidemics might be brought together with the emerging research area of bioarchaeology of impairment/disability to better understand the impact of epidemics and pandemics in the past.
Considering individuals with evidence for infectious disease as “survivors” is not new in palaeopathology. For any evidence of disease to manifest in the skeleton, the individual must have had that condition for a relatively prolonged time, long enough for skeletal changes to develop. So by definition, by the time paleopathologists can observe evidence for skeletal disease, they are also observing a “survivor.” Moving forward, we should also remember that some of these individuals are survivors of larger epidemics and therefore part of larger survivor cohorts. This expanded understanding of epidemic repercussions will allow survivor experiences and stories to be better contextualized within larger social health scenarios. By incorporating work from disability studies with our bioarchaeological understandings, we have the potential to conceptualize our interpretations a little differently—perhaps providing fuller interpretations of individual and group experiences of disease events, moving beyond individual-level experiences to see individuals as part of larger groups impaired by waves of epidemic disease. A “survivor lens” thus not only moves us from mortality to morbidity, impairment, and disability but also aids in making the leap from physical impairment to social disability—and exploring the relationship between them. It redirects our focus from definitive diagnosis to possibilities and beyond individuals (osteobiography, bioarchaeology of personhood) and relations (bioarchaeology of care) to specific groups and structure.
A survivor lens on epidemics and pandemics, therefore, is a shift in perspective. We cannot prescribe a specific method or detailed approach here, because this will necessarily depend on the relevant biological and social context: the pathogen and its associated disease(s), the time and place, and so on. Moving forward with this research, the next steps will include applying this theory using various methodological approaches. This operationalization might require the development of new techniques, creative applications of old approaches, and/or the continued integration of interdisciplinary methods. Regardless of the methods used, the point is that we must first work to think differently about the impact of epidemics. Specifically, we argue for a focus not only on the lasting impacts of deaths (e.g., on the economy or ecology), but also on the lasting impacts of sickness and impairment/disability at the group level as well as on the individual in context. While this is certainly not entirely new in bioarchaeology, there is ample room for further development—particularly with a multi- or transdisciplinary approach informed by disability theory. By taking a survivor lens on epidemic infectious disease, we can both better understand past outbreaks and their lasting impacts, as well as contribute to building a bioarchaeology of impairment and disability that is strengthened by engagement with the emerging historical work in this area. Furthermore, by better characterizing and contextualizing past survivor cohorts, we can provide a long history of the lives, roles, and contributions of disabled people, informing—and drawing attention to—the potential social and physical impacts of and on epidemic survivors. In doing so, the resulting new knowledge will affect understandings of the past in ways that can contribute importantly to wider conversations about disability and infectious disease in human history and inform present and future action.
References Cited
Adamson, J. D., J. P. Moody, A. F. W. Peart, R. A. Smillie, J. C. Wilt, and W. J. Wood. 1949. Poliomyelitis in the Arctic. Journal of the Canadian Medical Association 61(4):339–348.
Altenbaugh, Richard J. 2015. The Last Children’s Plague: Poliomyelitis, Disability, and Twentieth-Century American Culture. Palgrave Macmillan, New York.
Architectural Barriers Act (ABA), U.S.C. 42. 1968. §§ 4151 et seq. https://www.dol.gov/agencies/oasam/centers-offices/civil-rights-center/dlms2-0600. Accessed June 22, 2021.
Battles, Heather. 2011. Towards engagement: Exploring the prospects for an integrated anthropology of disability. Vis-à-Vis: Explorations in Anthropology 11(1):107–124.
Battles, Heather T. 2019. In the shadow of war: The forgotten 1916 polio epidemic in New Zealand. In Bioarchaeology of Marginalized People, edited by Madeleine L. Mant and Alyson Jaagumägi Holland. Elsevier Academic Press, London, pp. 181–203.
Berner, Margit, Doris Pany-Kucera, Nives Doneus, Vladimír Sladek, Michelle Gamble, and Sabine Eggers. 2021. Challenging definitions and diagnostic approaches for ancient rare diseases: The case of poliomyelitis. International Journal of Paleopathology 33:113–127. DOI: 10.1016/j.ijpp.2021.04.003.
Boutin, Alexis T. 2016. Exploring the social construction of disability: An application of the bioarchaeology of personhood model to a pathological skeleton from ancient Bahrain. International Journal of Paleopathology 12:17–28. DOI: 10.1016/j.ijpp.2015.10.005.
Bramanti, B., N., Zedda, N. Rinaldo, and E. Gualdi-Russo. 2018. A critical review of anthropological studies on skeletons from European plague pits of different epochs. Scientific Reports 8:17655. DOI: 10.1038/s41598-018-36201-w.
Brewis, Alexandra, Amber Wutich, and Pardis Mahdavi. 2020. Stigma, pandemics, and human biology: Looking back, looking forward. American Journal of Human Biology 32:e23480. DOI: 10.1002/ajhb.23480.
Brothwell, Don. 1961. The palaeopathology of early British man: An essay on the problems of diagnosis and analysis. The Journal of the Royal Anthropological Institute of Great Britain and Ireland 91(2):318–344.
Bruno, Richard L. 2002. The Polio Paradox: Uncovering the Hidden History of Polio to Understand and Treat “Post-Polio Syndrome” and Chronic Fatigue. Warner Books, New York.
Buckingham, Jane. 2011. Writing histories of disability in India: Strategies of inclusion. Disability and Society 26(4):419–431. DOI: 10.1080/09687599.2011.567792.
Buick Motor Division. 1946. Buick’s special driving controls for disabled veterans of World War II. Smithsonian Institution. https://americanhistory.si.edu/sites/default/files/1946%20Buick%20Valiant%20Catalog.pdf. Accessed June 23, 2021.
Buikstra, Jane E., and Charlotte A. Roberts, eds. 2012. The Global History of Palaeopathology: Pioneers and Prospects. Oxford University Press, Oxford.
Byrnes, Jennifer F., and Jennifer L. Muller. 2017. Bioarchaeology of Impairment and Disability: Theoretical, Ethnohistorical, and Methodological Perspectives. Springer, Cham.
Castells Navarro, Laura, William Southwell-Wright, Keith Manchester, and Jo Buckberry. 2017. Interpretation of a probable case of poliomyelitis in the Romano-British social context. Archaeological Review from Cambridge 32(1):34–52.
Castex, Dominique, and Sacha Kacki. 2016. Demographic patterns distinctive of epidemic cemeteries in archaeological samples. In Paleomicrobiology of Humans, edited by Michel Drancourt and Didiet Raoult. ASM Press, Washington, D.C., pp. 1–11. DOI: 10.1128/microbiolspec.PoH-0015-2015.
Chouinard, Vera. 1997. Making space for disabling difference: Challenging ableist geographies. Environment and Planning D: Society and Space 15:379–387.
Ciesielska, Joanna A., and Robert J. Stark. 2020. Possible neurogenic disorder in a female buried in the monastic cemetery at Ghazali (ca. 670–1270 CE), northern Sudan. International Journal of Osteoarchaeology 30(1):33–42. DOI: 10.1002/oa.2828.
Clark, Danielle V., Hannah Kibuuka, Monica Millard, Salim Wakabi, Luswa Lukwago, Alison Taylor, et al. 2015. Long-term sequelae after Ebola virus disease in Bundibugyo, Uganda: A retrospective cohort study. The Lancet Infectious Diseases 15(8):905–912. DOI: 10.1016/S1473-3099(15)70152-0.
Coryllos, P. M. 1933. How do rest and collapse treatment cure pulmonary tuberculosis? JAMA 100(7):480–482. DOI: 10.1001/jama.1933.02740070018006.
Cross, Morag. 1999. Accessing the inaccessible: Disability and archaeology. Archaeological Review from Cambridge 15(2):7–30.
Danforth, Scot. 2018. Becoming the Rolling Quads: Disability politics at the University of California, Berkeley, in the 1960s. History of Education Quarterly 58(4):506–536. DOI: 10.1017/heq.2018.29.
Darton, Yves, Isabelle Richard, and Marie-Cécile Truc. 2013. Osteomyelitis variolosa: A probable mediaeval case combined with unilateral sacroiliitis. International Journal of Paleopathology 3(4):288–293. DOI: 10.1016/j.ijpp.2013.05.008.
de Melo, Fernado Lucas, Joana Carvalho Moreira de Mello, Ana Maria Fraga, Kelly Nunes, and Sabine Eggers. 2010. Syphilis at the crossroad of phylogenetics and paleopathology. PLoS Neglected Tropical Diseases 4(1):e575. DOI: 10.1371/journal.pntd.0000575.
Dettwyler, K. A. 1991. Can palaeopathology provide evidence for “compassion”? American Journal of Physical Anthropology 84:375–384.
DeWitte, Sharon N. 2009. The effect of sex on risk of mortality during the Black Death in London, A.D. 1349–1350. American Journal of Physical Anthropology 139(2):222–234. DOI: 10.1002/ajpa.20974
DeWitte, Sharon N. 2010. Age patterns of mortality during the Black Death in London, A.D. 1349–1350. Journal of Archaeological Science 37(12):3394–3400. DOI: 10.1016/j.jas.2010.08.006.
DeWitte, Sharon N. 2014. The anthropology of plague: Insights from bioarcheological analyses of epidemic cemeteries. The Medieval Globe 1(1):Article 6. https://scholarworks.wmich.edu/tmg/vol1/iss1/6.
DeWitte, Sharon N., and James W. Wood. 2008. Selectivity of Black Death mortality with respect to preexisting health. Proceedings of the National Academy of Sciences 105(5):1436–1441. DOI: 10.1073/pnas.0705460105.
Disabled Peoples’ International (DPI). 1981. Proceedings of the First World Congress. DPI, Singapore.
Dittmer, D. K., and R. Teasell. 1993. Complications of immobilization and bed rest. Part 1: Musculoskeletal and cardiovascular complications. Canadian Family Physician 39:1428.
Dowling, Peter J. 1997. “A Great Deal of Sickness”: Introduced Diseases among the Aboriginal People of Colonial Southeast Australia [Ph.D. thesis]. The Australian National University, Canberra. DOI: 10.25911/5d7a27033fdfa.
Eichner, M., K. Hedeler, and K. Dietz. 1994. Stochastic models for the eradication of poliomyelitis: Minimum population size for polio virus persistence. In Models for Infectious Human Diseases, edited by V. Ishram and G. Medley. Cambridge University Press, Cambridge, pp. 315–327.
Evans, Alfred S. 1984. Viral Infections of Humans. 2nd ed. Plenum, New York.
Finlay, Nyree, ed. 1999. Disability and Archaeology. Vol. 15. The Department of Archaeology, Cambridge.
Fratamico, Pina M., James L. Smith, and Kim A. Bogden. 2009. Concluding perspectives of sequelae and long-term consequences of infectious diseases—what’s next? In Sequelae and Long-Term Consequences of Infectious Disease, edited by Pina M. Fratamico, James L. Smith, and Kim A. Brogden. ASM Press, Washington, D.C., pp. 487–493.
Fuentes, Agustín. 2020. A (bio)anthropological view of the COVID-19 era midstream: Beyond the infection. Anthropology Now 12(1):24–32. DOI: 10.1080/19428200.2020.1760635.
Gallagher, Hugh Gregory. 1998. Black Bird Fly Away: Disabled in an Able-Bodied World. Vandamere Press, Arlington, VA.
Gładykowska-Rzeczycka, J. J., and A. Śmiszkiewicz-Skwarska. 1998. Probable poliomyelitis from XVII-XVIII century cemetery in Poland. Journal of Paleopathology 10(1):5–12.
Godde, Kanya, Valerie Pasillas, and America Sanchez. 2020. Survival analysis of the Black Death: Social inequality of women and the perils of life and death in Medieval London. American Journal of Physical Anthropology 173(1):168–178. DOI: 10.1002/ajpa.24081.
Gowland, Rebecca. 2017. Embodied identities in Roman Britain: A bioarchaeological approach. Britannia 48:177–194.
Grauer, Anne L., and Charlotte A. Roberts. 2019. Fungal, viral, multicelled parasitic, and protozoan infections. In Ortner’s Identification of Pathological Conditions in Human Skeletal Remains, edited by Jane E. Buikstra. 3rd ed. Academic Press, New York, pp. 441–478.
Greenstein, Robert J., Thomas P. Gillis, David S. Scollard, and Sheldon T. Brown. 2009. In Sequelae and Long-Term Consequences of Infectious Disease, edited by Pina M. Fratamico, James L. Smith, and Kim A. Brogden. ASM Press, Washington, D.C., pp. 135–167.
Hatzenbuehler, Mark L., Jo C. Phelan, and Bruce G. Link. 2013. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health 103(5):813–821. DOI: 10.2105/AJPH.2012.301069.
Hawkey, Dianne E. 1998. Disability, compassion and the skeletal record: Using musculoskeletal stress markers (MSM) to construct an osteobiography from early New Mexico. International Journal of Osteoarchaeology 8:326–340. DOI: 10.1002/(SICI)1099-1212(1998090)8:5<326::AID-OA437>3.0.CO;2-W.
Hayashi, Shizu, Richard G. Hegele, and James C. Hogg. 2009. Latent viral infections. In Sequelae and Long-Term Consequences of Infectious Disease, edited by Pina M. Fratamico, James L. Smith, and Kim A. Brogden. ASM Press, Washington, D.C., pp. 339–369.
Holland, Daniel. 2006. Franklin D. Roosevelt’s Shangri‐La: Foreshadowing the Independent Living Movement in Warm Springs, Georgia, 1926–1945. Disability & Society 21(5):513–535. DOI: 10.1080/09687590600785993.
Honigsbaum, Mark, and Lakshmi Krishnan. 2020. Taking pandemic sequelae seriously: From the Russian influenza to COVID-19 long-haulers. The Lancet 396(10260):1389–1391. DOI: 10.1016/S0140-6736(20)32134-6.
Hubert, Jane, ed. 2000. Madness, Disability and Social Exclusion: The Archaeology and Anthropology of ‘Difference’. Routledge, London.
Hurst, Rachel. 2005. Disabled Peoples’ International: Europe and the social model of disability. In The Social Model of Disability: Europe and the Majority World, edited by C. Barnes and G. Mercer. The Disability Press, Leeds, pp. 65–79.
James, Peter Bai, Jonathan Wardle, Amie Steel, and Jon Adams. 2020. An assessment of Ebola-related stigma and its association with informal healthcare utilisation among Ebola survivors in Sierra Leone: A cross-sectional study. BMC Public Health 20(1):1–12. DOI: 10.1186/s12889-020-8279-7.
John, Chandy C., Paul Bangirana, Justus Byarugaba, Robert O. Opoka, Richard Idro, Anne M. Jurek, et al. 2008. Cerebral malaria in children is associated with long-term cognitive impairment. Pediatrics 122(1):e92–e99. DOI: 10.1542/peds.2007-3709.
Jorba, Jaume, Ray Campagnoli, Lina De, and Olen Kew. 2008. Calibration of multiple poliovirus molecular clocks covering an extended evolutionary range. Journal of Virology 82(9):4429–4440. DOI: 10.1128/JVI.02354-07.
Jubelt, Burk, and James C. Agre. 2000. Characteristics and management of postpolio syndrome. Journal of the American Medical Association 284(4):412–414. DOI: 10.1001/jama.284.4.412.
Kacki, Sacha, and Dominique Castex, D. 2014. La sépulture multiple de la basilique des Saints Martyrs Just et Pastor: Bio-archéologie des restes humains. Quaderns d’Arqueologia i Història de la Ciutat Barcelona 10:180–199.
Kaufert, Patricia Leyland, and Joseph M. Kaufert. 1984. Methodological and conceptual issues in measuring the long term impact of disability: The experience of poliomyelitis patients in Manitoba. Social Science and Medicine 19(6):609–618. DOI: 10.1016/0277-9536(84)90227-2.
Klausner, Jeffrey D., and Alexandra H. Freeman. 2009. Sequelae and long-term consequences of syphilis infection. In Sequelae and Long-Term Consequences of Infectious Disease, edited by Pina M. Fratamico, James L. Smith, and Kim A. Brogden. ASM Press, Washington, D.C., pp. 187–204.
Knudson, Kelly J., and Christopher M. Stojanowski. 2008. New directions in bioarchaeology: Recent contributions to the study of human social identities. Journal of Archaeological Research 16(4):397–432.
Knüsel, Christopher J., Zoë C. Chundun, and Peter Cardwell. 1992. Slipped proximal femoral epiphysis in a priest from the medieval period. International Journal of Osteoarchaeology 2:109–119.
Koven, S. 1994. Remembering and dismemberment: Crippled children, wounded soldiers, and the Great War in Great Britain. American Historical Review (October):1167–1202.
Kozlowski, T., and J. Piontek. 2000. A case of atrophy of bones of the right lower limb of a skeleton from a medieval (12th–14th centuries) burial ground in Gruczno, Poland. Journal of Paleopathology 12:5–16.
Kudlick, Catherine. 2013. Comment: On the borderland of medical and disability history. Bulletin of the History of Medicine 87(4):540–559. https://www.jstor.org/stable/26305959
Kudlick, Catherine. 2014. Smallpox, disability, and survival in nineteenth-century France: Rewriting paradigms from a new epidemic script. In Disability Histories, edited by Susan Burch and Michael Rembis. University of Illinois Press, Champaign, pp. 185–200.
Kudlick, Catherine. 2018. Social history of medicine and disability history. In The Oxford Handbook of Disability History (online version), edited by Michael Rembis, Catherine Kudlick, and Kim E. Nielsen. Oxford University Press, Oxford. DOI: 10.1093/oxfordhb/9780190234959.013.1.
Kuge, S., N. Kawamura, and A. Nomoto. 1989. Strong inclination toward transition mutation in nucleotide substitutions by poliovirus replicase. Journal of Molecular Biology 207:175–182.
László, Orsolya. 2017. A case of neurogenic paralysis from Tomb Kampp -43-, Thebes, Egypt. In Now Behold My Spacious Kingdom: Studies Presented to Zoltán Imre Fábián on the Occasion of His 63th Birthday, edited by Bori Németh. L’Harmattan Kiadó, Budapest, pp. 69–81.
Liebenberg, Gillian. 1994. Disease and Disability: Poliomyelitis, Rehabilitation and Social Reform for Disabled Persons in New Brunswick, 1941–1955 [Master’s thesis]. University of New Brunswick, Fredericton.
Linker, Beth. 2013. On the borderland of medical and disability history: A survey of the fields. Bulletin of the History of Medicine 87(4):499–535. DOI: 10.1353/bhm.2013.0074.
Llewellyn, A., and K. Hogan. 2000. The use and abuse of models of disability. Disability and Society 15(1):157–165. DOI: 10.1080/09687590025829.
Málaga, Martha R. Palma, and Krzysztof Makowski. 2019. Bioarchaeological evidence of care provided to a physically disabled individual from Pachacamac, Peru. International Journal of Paleopathology 25:139–149. DOI: 10.1016/j.ijpp.2018.08.002.
Mansukoski, Liina, and Vitale Stefano Sparacello. 2018. Smaller long bone cross-sectional size in people who died of tuberculosis: Insights on frailty factors from a 19th and early 20th century Finnish population. International Journal of Paleopathology 20:38–44. DOI: 10.1016/j.ijpp.2017.12.005.
Mant, Madeleine, Carlina de la Cova, and Megan B. Brickley. 2021. Intersectionality and trauma analysis in bioarchaeology. American Journal of Physical Anthropology 174(4):583–594. DOI: 10.1002/ajpa.24226.
Matczak, Magdalena, Jane E. Buikstra, J. Pearson, and A. M. Wyrwa. 2019. Bioarcheologia niepełnosprawności: przegląd obecnych badań i perspektywy na przyszłość [The bioarchaeology of disability: Review of current research and prospects for the future]. Museion Poloniae Maioris 6:35–57.
Mitchell, John K. 1900. Study of a mummy affected with anterior poliomyelitis. Transactions of the Association of American Physicians 15:134–136.
Moses, S. H. 1948. Report on the epidemic of anterior poliomyelitis in the Nicobar Islands. Indian Medical Gazette 83:355–563.
Nielsen, Nete Munk, Klaus Rostgaard, Knud Juel, Dorthe Askgaard, and Peter Aaby. 2003. Long-term mortality after poliomyelitis. Epidemiology 14(3):355–360. http://www.jstor.org/stable/3703858
Novak, Mario, Mislav Čavka, and Mario Šlaus. 2014. Two cases of neurogenic paralysis in medieval skeletal samples from Croatia. International Journal of Paleopathology 7:25–32. DOI: 10.1016/j.ijpp.2014.06.002.
Ohtake, Patricia J., Alan C. Lee, Jacqueline Coffey Scott, Rana S. Hinman, Naeem A. Ali, Carl R. Hinkson, et al. 2018. Physical impairments associated with post-intensive care syndrome: Systematic review based on the World Health Organization’s International Classification of Functioning, Disability and Health framework. Physical Therapy and Rehabilitation Journal 98(8):631–645. DOI: 10.1093/ptj/pzy059.
Oliver, Mike. 1996. Defining impairment and disability: Issues at stake. In Exploring the Divide: Illness and Disability, edited by Colin Barnes and Geof Mercer. The Disability Press, Leeds, pp. 29–54.
Patterson, Lindsey. 2012. Points of access: Rehabilitation centers, summer camps, and student life in the making of disability activism, 1960–1973. Journal of Social History 46(2):473–499. DOI: 10.1093/jsh/shs099.
Paul, John R. 1971. A History of Poliomyelitis. Yale University Press, New Haven, CT.
Perego, Elisa, Felicity Callard, Laurie Stras, Barbara Melville-Jóhannesson, Rachel Pope, and Nisreen A. Alwan. 2020. Why the patient-made term ‘Long Covid’ is needed. Wellcome Open Research 5:224. DOI: 10.12688/wellcomeopenres.16307.1.
Ramlow, Jonathan, Michael Alexander, Ronald LaPorte, Caroline Kaufmann, and Lewis Kuller. 1992. Epidemiology of the post-polio syndrome. American Journal of Epidemiology 136(7):769–786. DOI: 10.1093/aje/136.7.769.
Rembis, Michael. 2019. Challenging the impairment/disability divide. In Routledge Handbook of Disability Studies, edited by Nick Watson and Simo Vehmas. 2nd ed. Routledge, London, pp. 377–390.
Rico-Hesse, Rebeca, Mark A. Pallansch, Baldev K. Nottay, and Olen M. Kew. 1987. Geographic distribution of wild poliovirus type 1 genotypes. Virology 160:311–322. DOI: 10.1016/0042-6822(87)90001-8.
Rigeade, Catherine, Bruno Bizot, Anne Le Bot-Helly, and Michel Signoli. 2009. Une sépulture de pestiférés du Haut Moyen Âge à Vienne (Isère). Archéologie du Midi médiéval 27:19–29.
Roberts, C. A. 2011. The bioarchaeology of leprosy and tuberculosis: A comparative study of perceptions, stigma, diagnosis, and treatment. In Social Bioarchaeology, edited by Sabrina C. Agarwal and Bonnie A. Glencross. Wiley-Blackwell, Chichester, pp. 252–281. DOI: 10.1002/9781444390537.ch9.
Roberts, Charlotte. 1999. Disability in the skeletal record: Assumptions, problems and some examples. Archaeological Review from Cambridge 15(2):79–98.
Roberts, Charlotte A. 2000. Did they take sugar: The use of skeletal evidence in the study of disability in past populations. In Madness, Disability and Social Exclusion: The Archaeology and Anthropology of ‘Difference,’ edited by Jane Hubert. Routledge, London, pp. 46–59.
Roberts, Charlotte A. 2020. Leprosy: Past and Present. University of Florida Press, Gainesville.
Roberts, Charlotte A., and Jane E. Buikstra. 2019. Bacterial infections. In Ortner’s Identification of Pathological Conditions in Human Skeletal Remains, edited by Jane E. Buikstra. 3rd edition. Academic Press, New York, pp. 321–439.
Robbins Schug, Gwen. 2016. Begotten of corruption? Bioarchaeology and “othering” of leprosy in South Asia. International Journal of Paleopathology 15:1–9. DOI: 10.1016/j.ijpp.2016.09.002.
Ross, Jean C. 1993. A History of Poliomyelitis in New Zealand [Master’s thesis]. University of Canterbury, Canterbury, New Zealand.
Rothman, Juliet C. 2010. The challenge of disability and access: Reconceptualizing the role of the medical model. Journal of Social Work in Disability and Rehabilitation 9(2):194–222. DOI: 10.1080/1536710X.2010.493488.
Schrader, Sarah A., and Christina Torres-Rouff. 2020. Embodying bioarchaeology: Theory and practice. In Theoretical Approaches in Bioarchaeology, edited by Colleen M. Cheverko, Julia R. Prince-Buitenhuys, and Mark Hubbe. Routledge, London, pp. 15–27.
Schrenk, Alecia A., and Debra L. Martin. 2017. Applying the Index of Care to the case study of a Bronze Age teenager who lived with paralysis: Moving from speculation to strong inference. In New Developments in the Bioarchaeology of Care, edited by Lorna Tilley and Alecia A. Schrenk. Springer, Cham, pp. 47–64.
Semba, Richard D. 2003. The ocular complications of smallpox and smallpox immunization. Archives of Ophthalmology 121(5):715–719. DOI: 10.1001/archopht.121.5.715.
Shakespeare, Tom. 1999. Commentary: Observations on disability and archaeology. Archaeological Review from Cambridge 15(2):99–101.
Shakespeare, Tom. 2012. Still a health issue. Disability and Health Journal 5(3):129–131. DOI: 10.1016/j.dhjo.2012.04.002.
Shakespeare, Tom. 2014. Disability Rights and Wrongs Revisited. Routledge, New York.
Shuttleworth, Russell, and Helen Meekosha. 2017. Accommodating critical disability studies in bioarchaeology. In Bioarchaeology of Impairment and Disability, edited by Jennifer F. Byrnes and Jennifer L. Muller. Springer, Cham, pp. 19–38.
Signoli, Michel, Stephan Tzortzis, Bruno Bizot, Yann Ardagna, Catherine Rigeade, and Isabelle Séguy. 2007. Découverte d’un cimetière de pestiférés du xviie siècle (Puy-Saint-Pierre, Hautes-Alpes, France). In Peste: Entre épidémies et sociétés, edited by Michel Signoli, Dominique Chevé, Pascal Adalian, Gilles Boëtsch, and Olivier Dutour. Firenze University Press, Firenze, pp. 131–135. DOI: 10.36253/978-88-8453-489-7.
Smallman-Raynor, M. R., A. D. Cliff, B. Trevelyan, C. Nettleton, and S. Sneddon. 2006. Poliomyelitis: A World Geography. Emergence to Eradication. Oxford University Press, Oxford.
Sneed, D. 2020. The architecture of access: Ramps at ancient Greek healing sanctuaries. Antiquity 94(376):1015–1029. DOI: 10.15184/aqy.2020.123
Snyder, Sharon, and David Mitchell. 2006. Afterword—regulated bodies: Disability studies and the controlling professions. In Social Histories of Disability and Deformity, edited by David M. Turner and Kevin Stagg. Routledge, Oxon, pp. 175–189.
Snyder, Sharon L., and David T. Mitchell. 2010. Cultural Locations of Disability. University of Chicago Press, Chicago.
Sofaer, Joanna. R. 2006. The Body as Material Culture: A Theoretical Osteoarchaeology. Cambridge University Press, Cambridge.
Solari, Ana, Sérgio F. S. M. da Silva, Anne Marie Pessis, Gabriela Martin, and Niede Guidon. 2020. Applying the Bioarchaeology of Care model to a severely diseased infant from the Middle Holocene, north‐eastern Brazil: A step further into research on past health‐related caregiving. International Journal of Osteoarchaeology 30(4):482–491. DOI: 10.1002/oa.2876.
Southwell-Wright, William. 2013. Past perspectives: What can archaeology offer disability studies? In Emerging Perspectives on Disability Studies, edited by Matthew Wappett and Katrina Arndt. Palgrave Macmillan, New York, pp. 67–95.
Sparacello, Vitale Stefano, Charlotte A. Roberts, Alessandro Canci, Jacopo Moggi-Cecchi, and Damiano Marchi. 2016. Insights on the paleoepidemiology of ancient tuberculosis from the structural analysis of postcranial remains from the Ligurian Neolithic (northwestern Italy). International Journal of Paleopathology 15:50–64. DOI: 10.1016/j.ijpp.2016.08.003.
Spyrou, Maria A., Marcel Keller, Rezeda I. Tukhbatova, Christiana L. Scheib, Elizabeth A. Nelson, Aida Andrades Valtueña, et al. 2019. Phylogeography of the second plague pandemic revealed through analysis of historical Yersinia pestis genomes. Nature Communications 10:4470. DOI: 10.1038/s41467-019-12154-0.
Stodder, Ann L. W. 2017. Quantifying impairment and disability in bioarchaeological assemblages. In Bioarchaeology of Impairment and Disability, edited by Jennifer F. Byrnes and Jennifer L. Muller. Springer, Cham, pp. 183–200.
Teasell, R., and D. K. Dittmer. 1993. Complications of immobilization and bed rest. Part 2: Other complications. Canadian Family Physician 39:1440.
Tesini, Brenda L. 2020. Congenital syphilis. MSD Manual (Professional Version). Merck Sharp and Dohme Corp. https://www.msdmanuals.com/en-nz/professional/pediatrics/infections-in-neonates/congenital-syphilis. Accessed January 17, 2021.
Thompson, Andrew R. 2014. Differential diagnosis of limb length discrepancy in a 19th century burial from Southwest Mississippi. International Journal of Osteoarchaeology 24:517–530. DOI: 10.1002/oa.2238.
Tilley, Lorna. 2012. The bioarchaeology of care. The SAA Archaeological Record 12(3):39–41.
Tilley, Lorna. 2015. Theory and Practice in the Bioarchaeology of Care. Springer, Cham.
Tilley, Lorna, and Tony Cameron. 2014. Introducing the Index of Care: A web-based application supporting archaeological research into health-related care. International Journal of Paleopathology 6:5–9. DOI: 10.1016/j.ijpp.2014.01.003.
Tilley, Lorna, and Kenneth Nystrom. 2019. A ‘cold case’ of care: Looking at old data from a new perspective in mummy research. International Journal of Paleopathology 25:72–81. DOI: 10.1016/j.ijpp.2018.08.001.
Tilley, Lorna, and Alecia A. Schrenk. 2017. New Developments in the Bioarchaeology of Care. Springer, Cham.
Tornberg, Anna, and Lars Jacobsson. 2018. Care and consequences of traumatic brain injury in Neolithic Sweden: A case study of ante mortem skull trauma and brain injury addressed through the bioarchaeology of care. International Journal of Osteoarchaeology 28(2):188–198. DOI: 10.1002/oa.2646.
Torres-Castro, Rodrigo, Lilian Solis-Navarro, Mercè Sitjà-Rabert, and Jordi Vilaró. 2021. Functional limitations post-COVID-19: A comprehensive assessment strategy. Archivos de Bronconeumologia 57(Suppl. 1):7–8. DOI: 10.1016/j.arbres.2020.07.025.
UPIAS and the Disability Alliance. 1975. Fundamental Principles of Disability. UPIAS, London.
Valerio, Fernanda, Daniel P. Whitehouse, David K. Menon, and Virginia F. J. Newcombe. 2020. The neurological sequelae of pandemics and epidemics. Journal of Neurology 268:2629–2655. DOI: 10.1007/s00415-020-10261-3.
Vargha, Dóra. 2018a. Polio across the Iron Curtain: Hungary’s Cold War with an Epidemic. Cambridge University Press, Cambridge. DOI: 10.1017/9781108355421
Vargha, Dóra. 2018b. Polio and disability in Cold War Hungary. In The Oxford Handbook of Disability History, edited by Michael Rembis, Catherine Kudlick, and Kim E. Nielsen. Oxford University Press, Oxford, pp. 1–17. DOI: 10.1093/oxfordhb/9780190234959.013.22.
Waldron, Tony. 2000. Hidden or overlooked? Where are the disadvantaged in the skeletal record? In Madness, Disability and Social Exclusion: The Archaeology and Anthropology of ‘Difference’, edited by Jane Hubert. Routledge, London, pp. 29–45.
Waldron, Tony. 2014. Crooked timber: The life of Calvin Wells (1908–1978). Journal of Medical Biography 22(2):82–89. DOI: 10.1177/0967772013479734.
Windebank, A. J., W. J. Litchy, J. R. Daube, L. T. Kurland, M. B. Codd, and R. Iverson. 1991. Late effects of paralytic poliomyelitis in Olmsted County, Minnesota. Neurology 41(4):501–507. DOI: 10.1212/WNL.41.4.501.
Winkler, E., and K. Großschmidt. 1988. A case of poliomyelitis from an early medieval cemetery at Georgenberg/Upper Austria. Ossa 13:191–205.
Wolbring, Gregor. 2008. The politics of ableism. Development 51:252–258. DOI: 10.1057/dev.2008.17.
Wolfe, Kathi. 2012. Disability rights group: 30 Years as a force for change. Disability Rights Education and Defense Fund (DREDF). https://dredf.org/disability-rights-group-30-years-as-a-force-for-change/. Accessed June 21, 2021.
Yaussy, Samantha L. 2019. The intersections of industrialization: Variation in skeletal indicators of frailty by age, sex, and socioeconomic status in 18th- and 19th-century England. American Journal of Physical Anthropology 170:116–130. DOI: 10.1002/ajpa.23881.
aAnthropology, School of Social Sciences, The University of Auckland, Auckland, Aotearoa, New Zealand
bDepartment of Sociology and Anthropology, Mount Royal University, Calgary, Alberta, Canada
*Correspondence to: Heather Battles, The University of Auckland, Private Bag 92019, Auckland 1142 Aotearoa, New Zealand
e-mail: h.battles@auckland.ac.nz